Rheumatology is a branch of medicine dedicated to the diagnosis and treatment of rheumatic diseases. It is a subspecialty of internal medicine and pediatrics. Conditions treated by rheumatologists include clinical problems in joints, soft tissues, inherited connective tissue diseases, vasculitis, and autoimmune diseases. This field is multidisciplinary in nature, which means it relies on close relationships with other medical specialties. The goal of rheumatologists is to discover the underlying cause of rheumatic disease and conduct research to find better treatment options.
Rheumatology has changed significantly over the past twenty years from a predominantly inpatient specialty with poorly effective treatments to a specialty based primarily on outpatients with targeted and evidence-based therapies. However, one fundamental problem remains, which is the difficulty in defining the scope of diseases included in this field.
An adequate understanding of the pathophysiological processes underlying rheumatic diseases has prompted the development of new drugs. Today, physicians have access not only to new biologics, but also to specific registries designed to assess the actual use of these agents and their optimal role in treatment protocols.
In addition, rheumatology offers diverse perspectives for both clinical and research. This field will undoubtedly develop even further in the future, as better disease assessment, improved science, the development of new biomarkers as well as the optimisation of drug use will help to address many challenges ahead.
There are more than 150 different types of rheumatic diseases, including:
OSTEOARTRIT
Osteoarthritis is the most common form of arthritis, affecting millions of people worldwide. It occurs when the protective cartilage that cushions the ends of bones wears away over time.
Although osteoarthritis can damage any joint, the disease most commonly affects the joints of the hands, knees, hips and spine.
Symptoms of osteoarthritis can usually be managed, although joint damage cannot be reversed. Physical activity, maintaining a healthy weight, and certain types of treatments can slow the progression of the disease and help overcome pain and improve joint function.
Symptoms:
Symptoms of osteoarthritis often develop slowly and worsen over time. Signs and symptoms of osteoarthritis include:
- Pain. Affected joints may ache during or after movement.
- Rigidity. Joint stiffness may be most noticeable on waking or after prolonged inactivity.
- Tenderness. The joint may be tender when gentle pressure is applied to or near it.
- Loss of flexibility. Possible loss of mobility in the joint in its full range of motion.
- Scraping sensation. It is possible to hear popping in the joint when moving.
- Bone spurs. Additional pieces of bone may form around the affected joint and feel like hard lumps.
- Swelling. This can be caused by inflammation of the soft tissues surrounding the joint.
Reasons:
Osteoarthritis occurs when the cartilage that cushions the ends of the bones in joints gradually wears away. Cartilage is a hard, slippery tissue that allows almost frictionless movement of the joints. Eventually, if the cartilage wears away completely, the bone will rub on the bone. But in addition to the destruction of cartilage, osteoarthritis affects the entire joint. It causes changes in the bone and deterioration of the connective tissues that hold the joint together and attach the muscles to the bone. It also causes inflammation of the lining of the joints.
Risk factors:
Factors that can increase the risk of osteoarthritis include:
- Older age. The risk of osteoarthritis increases with age.
- Gender. Women are more likely to develop osteoarthritis, although it is not clear why.
- Obesity. Carrying extra body weight contributes to osteoarthritis in several ways, and the more the weight, the greater the risk. Increased weight adds stress to weight-bearing joints, such as the hips and knees. In addition, fat tissue produces proteins that can cause harmful inflammation in and around the joints.
- Injuries to the joints. Injuries, such as those that occur in sports or from an accident, can increase the risk of osteoarthritis. Even injuries that occurred many years ago and seemingly healed can increase the risk of osteoarthritis.
- Repetitive stress on the joint. If a patient's job or the sport they play puts repetitive stress on a joint, that joint can eventually develop osteoarthritis.
- Genetics. Some people inherit a tendency to develop osteoarthritis.
- Bone deformities. Some people are born with deformed joints or defective cartilage.
- Some metabolic diseases. These include diabetes and a condition in which the body has too much iron (hemochromatosis).
Complications:
Osteoarthritis is a degenerative disease that worsens over time, often leading to chronic pain. Joint pain and stiffness can become severe enough to make daily tasks difficult. The pain can cause depression and sleep disturbances.
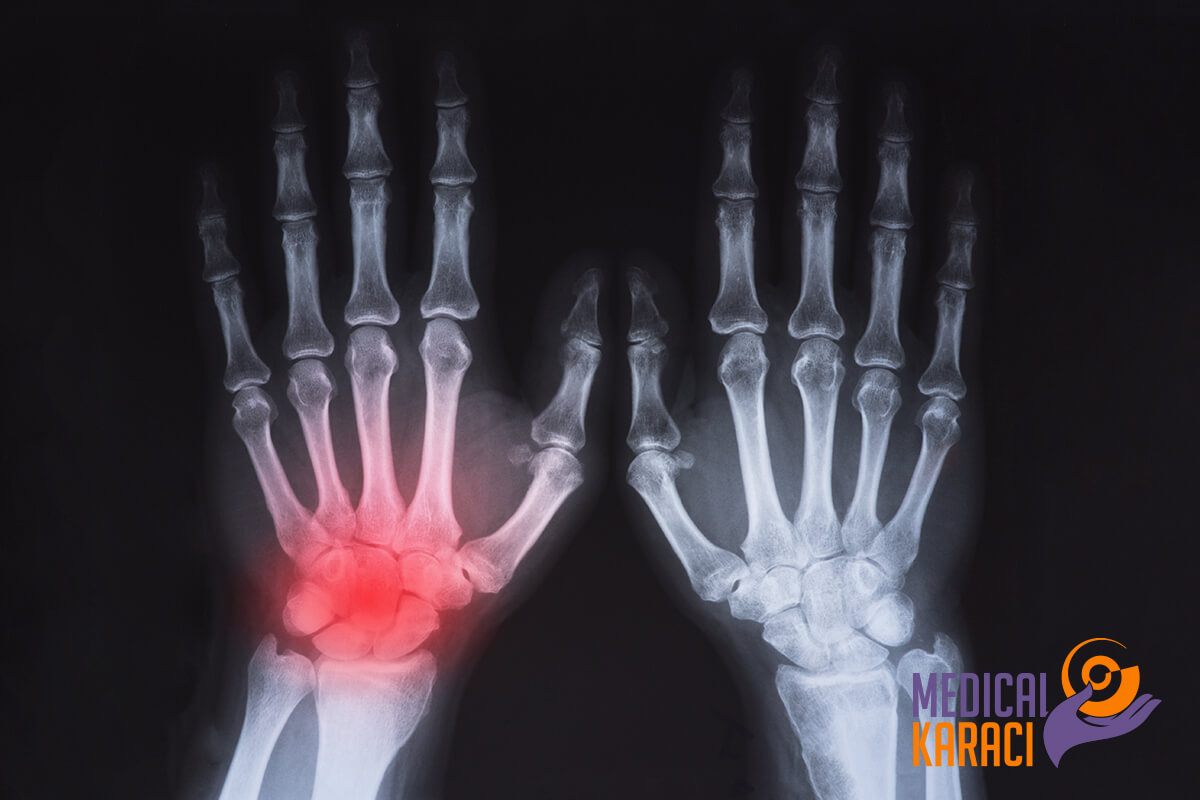
RHEUMATOID ARTHRITIS
Rheumatoid arthritis is a chronic inflammatory disease that can affect more than just the joints. In some people, the condition can damage a wide variety of bodily systems, including the skin, eyes, lungs, heart and blood vessels.
Rheumatoid arthritis is an autoimmune disorder and occurs when the immune system mistakenly attacks the body's tissues.
Unlike the wear-and-tear damage of osteoarthritis, rheumatoid arthritis affects the lining of the joints, causing painful swelling that can eventually lead to bone erosion and joint deformity.
The inflammation associated with rheumatoid arthritis can also damage other parts of the body. While new types of drugs have dramatically improved treatment options, severe rheumatoid arthritis can still cause serious damage.
Symptoms:
Signs and symptoms of rheumatoid arthritis may include:
- Tender, warm, swollen joints
- Joint stiffness, which usually worsens in the morning and after inactivity
- Fatigue, fever and loss of appetite
- Early rheumatoid arthritis usually affects the smaller joints - especially the metacarpophalangeal and metatarsal joints. As the disease progresses, symptoms often spread to the wrists, knees, ankles, elbows, hips and shoulders. In most cases, symptoms occur in the same joints symmetrically on both sides of the body.
About 40% of people who have rheumatoid arthritis also experience signs and symptoms that do not involve the joints. The signs and symptoms of rheumatoid arthritis can vary in severity and even come and go. Periods of increased disease activity, called flare-ups, alternate with periods of relative remission - when swelling and pain fade or disappear. Over time, rheumatoid arthritis can cause deformity and joint displacement.
Reasons:
Rheumatoid arthritis is an autoimmune disease. Normally, the immune system helps to protect the body from infection and disease. In rheumatoid arthritis, the immune system attacks the healthy tissues in the joints. It can also cause medical problems with the heart, lungs, nerves, eyes, and skin.
Doctors do not know how this process begins, although it seems likely that the cause is a genetic component. Although genes don't actually cause rheumatoid arthritis, they can make people more likely to react to environmental factors - such as infection with certain viruses and bacteria - that can trigger the disease.
Risk factors:
Factors that can increase the risk of rheumatoid arthritis include:
- Gender. Women are more likely than men to develop rheumatoid arthritis.
- Age. Rheumatoid arthritis can occur at any age, but most often begins in middle age.
- Family History. If a family member has rheumatoid arthritis, there may be an increased risk of the disease.
- Smoking. Smoking cigarettes increases the risk of developing rheumatoid arthritis, especially if there is a genetic predisposition to develop the disease. Smoking also appears to be associated with greater disease severity.
- Overweight. People who are overweight seem to be at a slightly higher risk of developing rheumatoid arthritis.
LUPUS
Lupus is an autoimmune disease that occurs when the body's immune system attacks its own tissues and organs. The inflammation caused by lupus can affect many different body systems - including the joints, skin, kidneys, blood cells, brain, heart and lungs.
Lupus can be difficult to diagnose because its signs and symptoms often mimic those of other diseases. The most distinctive sign of lupus - a rash on the face that looks like butterfly wings unfurling across both cheeks - is found in many, but not all, cases of lupus.
Some people are born with a tendency to develop lupus, which can be triggered by infections, certain medications or even sunlight. Although there is no cure for lupus, treatment can help control symptoms.
Symptoms:
No two cases of lupus are exactly the same. Signs and symptoms may appear suddenly or develop slowly, may be mild or severe, and may be temporary or permanent. Most people with lupus have a mild disease characterised by episodes - called flare-ups - when the signs and symptoms get worse for a while, then improve or even disappear completely for a while.
The signs and symptoms of lupus depend on which body systems are affected by the disease. The most common signs and symptoms include:
- Fatigue
- Fever
- Joint pain, stiffness and swelling
- A butterfly-shaped rash on the face that covers the cheeks and bridge of the nose or rashes elsewhere on the body
- Skin lesions that appear or worsen with sun exposure
- Fingers and toes that turn white or blue when exposed to cold or during stressful periods
- Shortness of breath
- Chest pain
- Dry eyes
- Headache, confusion and memory loss
Reasons:
As an autoimmune disease, lupus occurs when the immune system attacks healthy tissues in the body. Lupus is probably the result of a combination of genetics and environment. It seems that people with an inherited predisposition to lupus may develop the disease when they come into contact with something in the environment that can trigger lupus. However, the cause of lupus in most cases is unknown. Some potential triggering factors include:
- Sunlight. Exposure to the sun can cause lupus skin lesions or cause an internal reaction in susceptible people.
- Infections. The presence of an infection can initiate lupus or cause a relapse in some people.
- Medication. Lupus can be triggered by certain types of blood pressure medications, anti-seizure medications, and antibiotics. People who have medication-induced lupus usually get better when they stop taking the medicine. Rarely, symptoms may continue even after stopping the medicine.
Risk factors:
Factors that can increase the risk of lupus include:
- Gender. Lupus is more common in women.
- Age. Although lupus affects people of all ages, it is most commonly diagnosed between the ages of 15 and 45.
- Race. Lupus is more common in African Americans, Latinos, and Asian Americans.
Complications:
The inflammation caused by lupus can affect many areas of the body, including:
- Kidneys. Lupus can cause serious kidney damage, and kidney failure is one of the leading causes of death among people with lupus.
- Brain and central nervous system. If the brain is affected by lupus, there may be headaches, dizziness, behavioural changes, vision problems and even strokes or seizures. Many people with lupus experience memory problems and may have difficulty expressing their thoughts.
- Blood and blood vessels. Lupus can lead to blood problems, including a reduced number of healthy red blood cells (anemia) and an increased risk of bleeding or blood clotting. It can also cause inflammation of the blood vessels.
- Lungs. The presence of lupus increases the chances of developing inflammation of the lining of the chest cavity, which can make breathing painful. Bleeding in the lungs and pneumonia are also possible.
- Heart. Lupus can cause inflammation of the heart muscle, arteries, or heart membrane. The risk of heart disease and heart attacks also increases significantly.
Other types of complications:
The presence of lupus also increases the risk of:
- Infection. People with lupus are more vulnerable to infections because both the disease and its treatment can weaken the immune system.
- Cancer. The presence of lupus appears to increase the risk of cancer; however, the risk is small.
- Death of bone tissue. This occurs when the blood supply to the bone decreases, often leading to small fractures in the bone and eventually to bone collapse.
- Complications during pregnancy. Women with lupus have an increased risk of miscarriage. Lupus increases the risk of high blood pressure during pregnancy and preterm birth. To reduce the risk of these complications, doctors often recommend delaying pregnancy until the disease has been under control for at least six months.
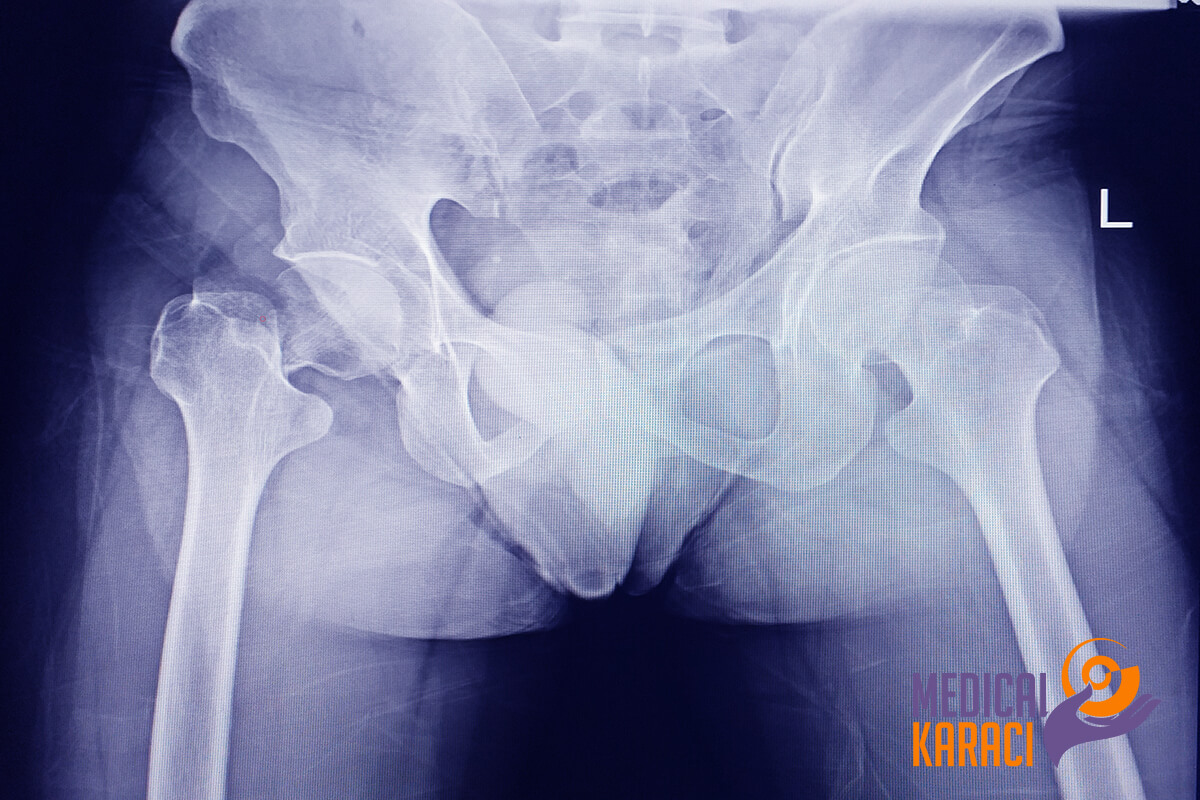
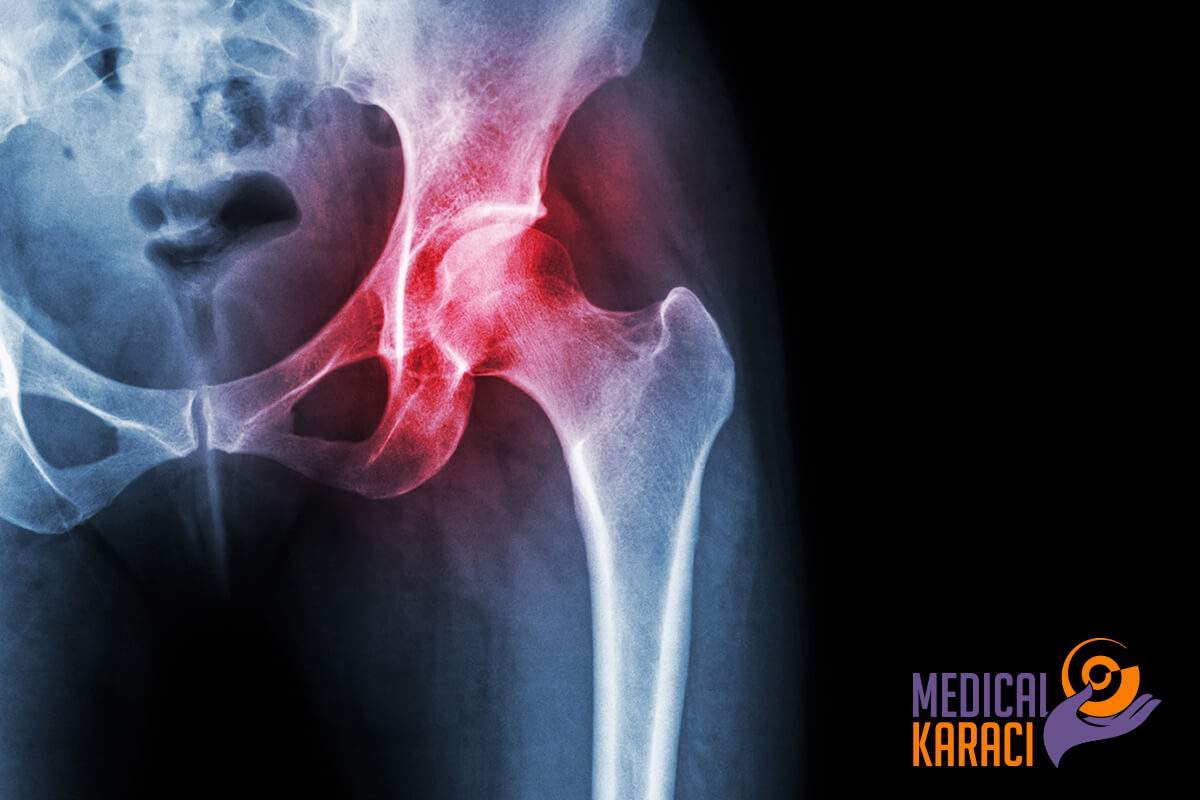
BECHTEREW'S DISEASE
Ankylosing spondylitis is an inflammatory disease that, over time, can lead to fusion of some of the vertebrae of the spine. This fusion makes the spine less flexible and can lead to a hunched posture. If the ribs are affected, breathing may become difficult.
Ankylosing spondylitis affects men more often than women. Signs and symptoms usually begin in early adulthood. Inflammation can also occur in other parts of the body - most commonly in the eyes.
There is no cure for ankylosing spondylitis, but treatment can relieve symptoms and possibly slow the progression of the disease.
Symptoms:
Early signs and symptoms of ankylosing spondylitis can include pain and stiffness in the lower back and hips, especially in the morning and after periods of inactivity. Neck pain and fatigue are also common. Over time, symptoms may worsen, improve or stop at irregular intervals.
The most commonly affected areas are:
- Sacroiliac joints-the joints between the base of the spine and the pelvis
- The vertebrae in the lower back
- The places where the tendons and ligaments attach to the bones, mainly in the spine but sometimes along the back of the heel
- The cartilage between the sternum and the ribs
- Hip and shoulder joints
Reasons:
Ankylosing spondylitis has no known specific cause, although genetic factors seem to be involved. In particular, people who have a gene called HLA-B27 are at significantly increased risk of developing ankylosing spondylitis. However, only some people with the gene develop the condition.
Complications:
In severe ankylosing spondylitis, new bone is formed as part of the body's attempts to heal itself. This new bone gradually bridges the gap between the vertebrae and eventually fuses parts of the vertebrae. These parts of the spine become rigid and inflexible. It can also stiffen the rib cage, limiting the capacity and function of the lungs.
Other complications may include:
- Eye inflammation (uveitis). One of the most common complications of ankylosing spondylitis, uveitis can cause rapid eye pain, sensitivity to light and blurred vision.
- Compression fractures. Some people's bones weaken during the early stages of ankylosing spondylitis. The weakened vertebrae can become crushed, increasing the severity of the hunched posture. Vertebral fractures can put pressure on and possibly injure the spinal cord and nerves that run through the spine.
- Heart problems. Ankylosing spondylitis can cause problems with the aorta, the largest artery in the body. The inflamed aorta can enlarge to the point that it distorts the shape of the aortic valve in the heart, impairing its function. The inflammation associated with ankylosing spondylitis increases the risk of heart disease in general.
SJÖGREN'S SYNDROME
Sjögren's syndrome is a disorder of the immune system identified by its two most common symptoms - dry eyes and dry mouth.
The condition often accompanies other immune system disorders, such as rheumatoid arthritis and lupus. In Sjögren's syndrome, the mucous and moisture-secreting glands of the eyes and mouth are usually affected first - leading to a decrease in tears and saliva.
Although Sjögren's syndrome can develop at any age, most people are over the age of 40 at the time of diagnosis. The condition is much more common in women. Treatment focuses on relieving symptoms.
Symptoms:
The two main symptoms of Sjögren's syndrome are:
- Dry eyes. Eyes may burn, itch, or feel gritty - as if there is sand in them.
- Dry mouth. The mouth may look like it is full of cotton, making it difficult to swallow or speak.
- Some people with Sjögren's syndrome also have one or more of the following complaints:
- Joint pain, swelling and stiffness
- Swollen salivary glands - especially the set located behind the jaw and in front of the ears
- Skin rashes or dry skin
- Vaginal dryness
- Persistent dry cough
- Prolonged fatigue
Reasons:
Sjögren's syndrome is an autoimmune disease- the immune system mistakenly attacks the body's own cells and tissues.
Scientists are not sure why some people develop Sjögren's syndrome. Certain genes put people at higher risk for the disease, but it seems that a trigger mechanism is needed - such as infection with a particular virus or strain of bacteria.
In Sjögren's syndrome, the immune system first targets the glands that produce tears and saliva. But it can also damage other parts of the body such as joints, thyroid, kidneys, liver, lungs, skin, nerves.
Risk factors:
Sjögren's syndrome usually occurs in people with one or more known risk factors, including:
- Age. Sjögren's syndrome is usually diagnosed in people over 40.
- Gender. Women are much more likely to develop Sjögren's syndrome.
- Rheumatic disease. It is common for people who have Sjögren's syndrome to also have a rheumatic disease - such as rheumatoid arthritis or lupus.
Complications:
The most common complications of Sjögren's syndrome involve the eyes and mouth:
- Dental cavities. Because saliva helps protect teeth from the bacteria that cause tooth decay, if the mouth is dry there is a tendency for tooth decay to develop.
- Infections. People with Sjögren's syndrome are much more likely to develop oral thrush, a fungal infection in the mouth.
- Vision problems. Dry eyes can lead to sensitivity to light, blurred vision and corneal damage.
Less common complications can affect:
- Lungs, kidneys or liver. Inflammation can cause pneumonia, bronchitis, or other problems in the lungs; lead to problems with kidney function; and cause hepatitis or cirrhosis in the liver.
- Lymph nodes. A small percentage of people with Sjögren's syndrome develop cancer of the lymph nodes (lymphoma).
- Nerves. Numbness and burning in the hands and feet (peripheral neuropathy) may develop.
PODAGRA
Gout is a common and complex form of arthritis that can affect any person. It is characterised by sudden, severe attacks of pain, swelling, redness and tenderness in one or more joints, most commonly in the big toe.
An attack of gout can occur suddenly, often waking you up in the middle of the night with the feeling that your big toe is on fire. The affected joint is hot, swollen and so tender that even the weight of the sheet on it can seem unbearable.
Gout symptoms may come and go, but there are ways to manage symptoms and prevent attacks.
Symptoms:
The signs and symptoms of gout almost always appear suddenly and often at night. They include:
- Intense pain in the joints. Gout usually affects the big toe, but can occur in any joint. Other commonly affected joints include the ankles, knees, elbows, wrists and fingers. The pain is likely to be worst in the first four to 12 hours after onset.
- Prolonged discomfort. After the worst pain subsides, joint discomfort can last from a few days to several weeks. Later attacks are likely to last longer and affect more joints.
- Inflammation and redness. The affected joint or joints become swollen, sensitive, warm and red.
- Limited range of movement. As gout progresses, joint mobility may be limited.
Reasons:
Gout occurs when urate crystals build up in the joint, causing inflammation and intense pain when it attacks. Urates crystals can form when there are high levels of uric acid in the blood. The body produces uric acid when it breaks down purines, substances that are found naturally in the body. Purines are also found in some foods, including red meat and organ meats such as liver. Purine-rich seafood includes anchovies, sardines, scallops, trout and tuna. Alcoholic beverages, especially beer, and beverages sweetened with fruit sugar (fructose) promote higher levels of uric acid.
Normally, uric acid dissolves in the blood and passes through the kidneys into the urine. But sometimes either the body produces too much uric acid or the kidneys excrete too little uric acid. When this happens, uric acid can build up, forming sharp, needle-shaped urate crystals in the joint or surrounding tissues that cause pain, inflammation, and swelling.
Risk factors:
It is more likely to develop gout if there are high levels of uric acid in the body. Factors that increase the level of uric acid in the body include:
- Diet. Eating a diet rich in red meat and shellfish and drinking beverages sweetened with fruit sugar (fructose) increase uric acid levels, which increases the risk of gout. Drinking alcohol, especially beer, also increases the risk of gout.
- Weight. When overweight, the body produces more uric acid and the kidneys have less time to eliminate uric acid.
- Medical Condition. Certain diseases and conditions increase the risk of gout. These include untreated high blood pressure and chronic conditions such as diabetes, obesity, metabolic syndrome, and heart and kidney disease.
- Certain drugs. Low doses of aspirin and some drugs used to control hypertension - including thiazide diuretics, angiotensin-converting enzyme (ACE) inhibitors and beta blockers - can also raise uric acid levels. The same can be said for the use of anti-rejection drugs prescribed to people who have undergone organ transplants.
- Family history of gout. If other family members have had gout, you are more likely to develop the disease.
- Age and gender. Gout occurs more often in men, mainly because women tend to have lower levels of uric acid. After menopause, however, uric acid levels in women approach those in men. Men are also more likely to develop gout earlier - usually between the ages of 30 and 50 - while women typically develop signs and symptoms after menopause.
- Recent surgery or trauma. Experiencing recent surgery or trauma can sometimes trigger a gout attack. In some people, getting a vaccination can trigger an attack of gout.
Complications:
People with gout can develop more severe conditions, such as:
- Recurrent gout. Some people may never experience signs and symptoms of gout again. Others may get gout several times each year. Medications can help prevent gout attacks in people with recurrent gout. If left untreated, gout can cause erosion and destruction of the joint.
- Advanced gout. Untreated gout can cause deposits of urate crystals to form under the skin in nodules called tophi (TOE-fie). Tophi can develop in several areas, such as the fingers, hands, feet, elbows or Achilles tendons along the back of the ankles. Tophi are usually not painful, but can become swollen and tender during gout attacks.
- Kidney stones. Urate crystals can collect in the urinary tract of people with gout, causing kidney stones. Medications can help reduce the risk of kidney stones.
SCLERODERMIA
Scleroderma is a group of rare diseases that involve hardening and tightening of the skin and connective tissue.
Scleroderma affects women more often than men and is most common between the ages of 30 and 50. Although there is no cure for scleroderma, various treatments can relieve symptoms and improve quality of life.
There are many different types of scleroderma. In some people, scleroderma only affects the skin. But in many people, scleroderma also damages structures outside the skin, such as blood vessels, internal organs and the digestive tract (systemic scleroderma). Signs and symptoms vary depending on what type of scleroderma it is.
Symptoms:
The signs and symptoms of scleroderma vary depending on which parts of the body are affected:
- Leather. Almost everyone who has scleroderma experiences hardening and tightening patches on the skin. These spots may be shaped like ovals or straight lines or cover wide areas of the body and extremities. The number, location and size of the patches vary depending on the type of scleroderma. The skin may appear shiny because it is so tight and movement of the affected area may be restricted.
- Fingers or toes. One of the earliest signs of systemic scleroderma is Raynaud's disease, which causes the small blood vessels in the fingers and toes to constrict in response to cold temperatures or emotional stress. When this happens, the fingers or toes may become blue, painful or numb. Raynaud's disease also occurs in people who do not have scleroderma.
- Digestive system. Scleroderma can cause different digestive symptoms, depending on which part of the digestive tract is affected. If the esophagus is affected, there may be heartburn or difficulty swallowing. If the intestines are affected, there may be cramping, bloating, diarrhea or constipation. Some people who have scleroderma may also have trouble absorbing nutrients if their intestinal muscles do not move food through the intestines properly.
- Heart, lungs or kidneys. Scleroderma can affect the function of the heart, lungs or kidneys to varying degrees. These problems, if left untreated, can become life-threatening.
Reasons:
Scleroderma results from overproduction and accumulation of collagen in body tissues. Collagen is a fibrous type of protein that makes up the connective tissue of the body, including the skin.
Doctors don't know exactly what causes the abnormal collagen production to start, but it seems that the body's immune system plays a role. Most likely, scleroderma is caused by a combination of factors, including immune system problems, genetics and environmental factors.
Risk factors:
Anyone can get scleroderma, but it occurs much more often in women than in men. Several combined factors seem to influence the risk of developing scleroderma:
- Genetics. People who have certain gene variations seem to be more likely to develop scleroderma. This may explain why a small number of scleroderma cases seem to occur in families and why certain types of scleroderma are more common in certain ethnic groups.
- Environmental Triggers. Research has shown that in some people the symptoms of scleroderma can be triggered by exposure to certain viruses, drugs or medications. Repeated exposure to certain harmful substances or chemicals, for example at work, can also increase the risk of scleroderma.
- Immune system problems. Scleroderma is thought to be an autoimmune disease. This means that it occurs in part because the body's immune system begins to attack connective tissues. In 15 to 20 percent of cases, a person who has scleroderma also has symptoms of another autoimmune disease, such as rheumatoid arthritis, lupus or Sjögren's syndrome.
Complications:
Complications of scleroderma range from mild to severe and can affect:
- Fingertips. Raynaud's disease, which occurs in systemic scleroderma, can be so severe that the restricted blood flow permanently damages the fingertip tissue, causing pitting or skin sores. In some cases, the fingertip tissue may die and require amputation.
- Lungs. Scarring of lung tissue can lead to decreased lung function, which can affect breathing and exercise tolerance. High blood pressure may also develop in the arteries to the lungs.
- Kidneys. When scleroderma affects the kidneys, increased blood pressure and an increased level of protein in the urine may develop. More serious consequences of kidney complications can include renal crisis, which involves a sudden rise in blood pressure and rapid kidney failure.
- Heart. Scarring of the heart tissue increases the risk of abnormal heartbeats and congestive heart failure and can cause inflammation of the membrane sac around the heart. Scleroderma can also increase the pressure in the right side of the heart and cause it to wear out.
- Teeth. Severe tightening of the facial skin can lead to a smaller and narrower mouth, which can make it difficult to brush your teeth or even have them professionally cleaned. People who have scleroderma often do not produce a normal amount of saliva, so the risk of tooth decay increases even more.
- Digestive system. Digestive problems associated with scleroderma can lead to heartburn and difficulty swallowing. It can also cause bouts of cramping, bloating, constipation or diarrhea.
- Sexual function. Men who have scleroderma may experience erectile dysfunction. Scleroderma can also affect women's sexual function by reducing sexual lubrication and shrinking the vaginal opening.
INFECTIOUS ARTHRITIS
Septic arthritis is a painful infection in the joint that can come from germs that pass through the blood from another part of the body. Septic arthritis can also occur when a penetrating injury, such as an animal bite or trauma, delivers germs directly to the joint.
Infants and the elderly are most likely to develop septic arthritis. People who have artificial joints are also at risk for septic arthritis. Knees are most commonly affected, but septic arthritis can also affect hips, shoulders and other joints. Infection can quickly and severely damage the cartilage and bone in the joint, so prompt treatment is critical.
Symptoms:
Septic arthritis usually causes extreme discomfort and difficulty using the affected joint. The joint may be swollen, red and warm and there may be fever.
If septic arthritis occurs in an artificial joint (prosthesis infection), signs and symptoms such as mild pain and swelling may develop months or years after knee or hip replacement surgery. Loosening of the joint may also occur, causing pain on movement or when straining the joint. Usually the pain goes away at rest. In extreme cases, the joint may dislocate.
Reasons:
Septic arthritis can be caused by bacterial, viral or fungal infections. Bacterial infection with Staphylococcus aureus is the most common cause. This bacterium usually lives even on healthy skin.
Septic arthritis can develop when an infection, such as a skin infection or urinary tract infection, spreads through the blood to the joint. Less commonly, a puncture wound, an injection of medicine or surgery in or near a joint - including joint replacement surgery - can lead to germs entering the joint space.
The lining of the joints has little ability to protect itself from infection. The body's response to infection - including inflammation, which can increase pressure and reduce blood flow to the joint - contributes to the damage.
Risk factors:
Risk factors for septic arthritis include:
- Existing joint problems. Chronic diseases and conditions that affect the joints-such as osteoarthritis, gout, rheumatoid arthritis, or lupus-can increase the risk of septic arthritis, as can previous joint surgeries and joint injuries.
- The presence of an artificial joint. Bacteria can be introduced during joint replacement surgery or an artificial joint can become infected if germs travel to the joint from a different area of the body through the bloodstream.
- Taking medicines for rheumatoid arthritis. People with rheumatoid arthritis have an extra increased risk due to the medications they take, which can suppress the immune system, making infections more likely. Diagnosing septic arthritis in people with rheumatoid arthritis is difficult as many of the signs and symptoms are similar.
- The fragility of the skin. Skin that breaks easily and heals poorly can give bacteria access to the body. Skin conditions such as psoriasis and eczema increase the risk of septic arthritis, as do infected skin wounds. People who regularly inject drugs also have a higher risk of injection site infection.
- Weak immune system. People with weak immune systems are at greater risk of septic arthritis. This includes people with diabetes, kidney and liver problems, and those who take medications that suppress their immune system.
- Joint trauma. Animal bites, puncture wounds or cuts on the joint can be a risk factor for the development of septic arthritis.
The presence of a combination of risk factors is a greater risk than the presence of a single risk factor.
Complications:
If treatment is delayed, septic arthritis can lead to joint degeneration and permanent damage.
Treatment involves draining the joint with a needle or during surgery. Antibiotics are also usually needed.
JUVENILE IDIOPATHIC ARTHRITIS
Juvenile idiopathic arthritis, formerly known as juvenile rheumatoid arthritis, is the most common type of arthritis in children under 16 years of age.
Juvenile idiopathic arthritis can cause constant joint pain, swelling and stiffness. Some children may only experience symptoms for a few months, while others have symptoms for many years.
Some types of juvenile idiopathic arthritis can cause serious complications, such as growth problems, joint damage and eye inflammation. Treatment focuses on controlling pain and inflammation, improving function and preventing disability.
Symptoms:
The most common signs and symptoms of juvenile idiopathic arthritis are:
- Pain. Although the child may not complain of joint pain, he or she may limp - especially in the morning or after rest.
- Swelling. Joint swelling is common, but is often first noticed in larger joints, such as the knee.
- Rigidity. The child may appear more clumsy than usual.
- Fever, swollen lymph nodes and rash. In some cases, fever, swollen lymph nodes or a rash on the body may occur.
- Juvenile idiopathic arthritis can affect one or many joints. There are several different subtypes of juvenile idiopathic arthritis, but the main ones are systemic, oligoarticular and polyarticular. Which type a child has depends on the symptoms, the number of joints affected and whether fever and rashes are hallmarks.
Like other forms of arthritis, juvenile idiopathic arthritis is characterized by periods when symptoms flare and times when symptoms may be minimal.
Reasons:
Juvenile idiopathic arthritis occurs when the body's immune system attacks its own cells and tissues. It is not known why this happens, but both heredity and environment seem to play a role.
Complications:
Several serious complications can result from juvenile idiopathic arthritis. But careful monitoring of the condition and seeking appropriate medical attention can significantly reduce the risk of these complications:
- Eye problems. Some forms can cause eye inflammation. If this condition is not treated, it can lead to cataracts, glaucoma and even blindness.
- Eye inflammation often proceeds without symptoms, so it is important that children with this condition are examined regularly by an ophthalmologist.
- Growth problems. Juvenile idiopathic arthritis can interfere with a child's bone growth and development. Some medications used for treatment, mainly corticosteroids, can also inhibit growth.
RHEUMATIC POLYMYALGIA
Rheumatic polymyalgia is an inflammatory disease that causes muscle pain and stiffness, especially in the shoulders and hips. The signs and symptoms of rheumatic polymyalgia usually start quickly and worsen in the morning.
Most people who develop rheumatic polymyalgia are over the age of 65. It rarely affects people under 50.
This condition is related to another inflammatory condition called giant cell arteritis. Giant cell arteritis can cause headaches, vision problems, jaw pain and scalp tenderness.
Symptoms:
Signs and symptoms of rheumatic polymyalgia usually occur on both sides of the body and may include:
- Shoulder pain
- Pain in the neck, upper arms, buttocks or thighs
- Stiffness in the affected areas, especially in the morning or after some time of inactivity
- Limited range of movement in affected areas
- Pain or stiffness in the wrists, elbows or knees
- There may also be more general signs and symptoms, including:
- Mild fever
- Fatigue
- General malaise
- Loss of appetite
- Unwanted weight loss
- Depression
Reasons:
The exact cause of rheumatic polymyalgia is unknown. Two factors seem to be involved in the development of this condition:
Genetics. Certain genes and gene variations can increase the risk of developing the disease.
Environmental exposure. New cases of rheumatic polymyalgia tend to come in cycles, possibly developing seasonally. This suggests that an environmental factor, such as a virus, may play a role. But no specific virus has been shown to cause rheumatic polymyalgia.
Giant cell arteritis:
Rheumatic polymyalgia and another disease known as giant cell arteritis share many similarities. Many people who have one of these diseases also have symptoms of the other.
Giant cell arteritis leads to inflammation of the lining of the arteries, most commonly the arteries in the temples. Signs and symptoms include headache, jaw pain, vision problems and scalp tenderness. If left untreated, this condition can lead to stroke or blindness.
Risk factors:
Risk factors for rheumatic polymyalgia include:
- Age. Rheumatic polymyalgia almost exclusively affects the elderly. Most often it occurs between 70 and 80 years.
- Gender. Women are about two to three times more likely to develop the disease.
- Race. Rheumatic polymyalgia is most common among white people whose ancestors are from Scandinavia or northern Europe.
Complications:
Symptoms of rheumatic polymyalgia can significantly affect the ability to perform everyday activities, such as getting out of bed, getting out of a chair or out of a car, combing hair or bathing, dressing. These difficulties can affect health, social interactions, physical activity, sleep and general well-being.
WASCULITE
Vasculitis involves inflammation of the blood vessels. Inflammation can lead to thickening of the blood vessel walls, which reduces the width of the passage through the vessel. If blood flow is restricted, this can lead to organ and tissue damage.
There are many types of vasculitis and most of them are rare. Vasculitis can affect only one or a few organs. The condition can be short-term or long-term.
Vasculitis can affect anyone, although some types are more common among certain age groups. Depending on the type, the condition may improve without treatment. Most types require medication to control inflammation and prevent flare-ups.
Symptoms:
Common signs and symptoms of most types of vasculitis include:
- Fever
- Headache
- Fatigue
- Weight Loss
Other signs and symptoms are related to the affected body parts, including:
- Digestive system. If the stomach or intestines are affected, there may be pain after eating. Ulcers and perforations are possible, which can lead to blood in the stool.
- Ears. Dizziness, tinnitus, and sudden hearing loss may occur.
- Eyes. Vasculitis can make the eyes look red and itch or burn. Giant cell arteritis can cause double vision and temporary or permanent blindness in one or both eyes. Sometimes this is the first sign of the disease.
- Hands or feet. Some types of vasculitis can cause numbness or weakness in the arm or leg. The palms of the hands and soles of the feet may swell or become stiff.
- Lungs. Shortness of breath or even coughing up blood can develop if vasculitis affects the lungs.
- Leather. Bleeding under the skin may manifest as red spots. Vasculitis can also cause lumps or open sores on the skin.
Reasons:
The exact cause of vasculitis is not fully understood. Some types are related to genetic makeup. Others result from the immune system attacking blood vessel cells by mistake. Possible triggers for this immune system reaction include:
- Infections such as hepatitis B and hepatitis C
- Cancer of the blood
- Diseases of the immune system, such as rheumatoid arthritis, lupus and scleroderma
- Reactions to certain medicines
- Risk factors
- Factors that can increase risk include:
- Age. Giant cell arteritis rarely occurs before the age of 50, while Kawasaki disease is most common in children under the age of 5.
- Family History. Behcet's disease, granulomatosis with polyangiitis, and Kawasaki disease have been associated with heredity.
- Lifestyle choices. Cocaine use may increase the risk of developing vasculitis. Tobacco smoking, especially if in men younger than 45 years, may increase the risk of Burger's disease.
- Medication. Vasculitis can sometimes be triggered by medications such as hydralazine, allopurinol, minocycline, and propylthiouracil.
- Infections. The presence of hepatitis B or C can increase the risk of vasculitis.
- Immune disorders. People who have disorders in which their immune system mistakenly attacks the body may be at higher risk for vasculitis. Examples include lupus, rheumatoid arthritis, and scleroderma.
- Gender. Giant cell arteritis is much more common in women, while Bürger's disease is more common in men.
Complications:
Complications of vasculitis depend on the type and severity of the condition. Or they may be related to side effects of the prescription drugs that are used to treat the condition. Complications of vasculitis include:
- Organ damage. Some types of vasculitis can be severe, causing damage to major organs.
- Blood clots and aneurysms. A blood clot can form in a blood vessel, obstructing blood flow. Rarely, vasculitis causes a blood vessel to weaken and bulge, forming an aneurysm.
- Loss of vision or blindness. This is a possible complication of untreated giant cell arteritis.
- Infections. Some of the drugs used to treat vasculitis can weaken the immune system.
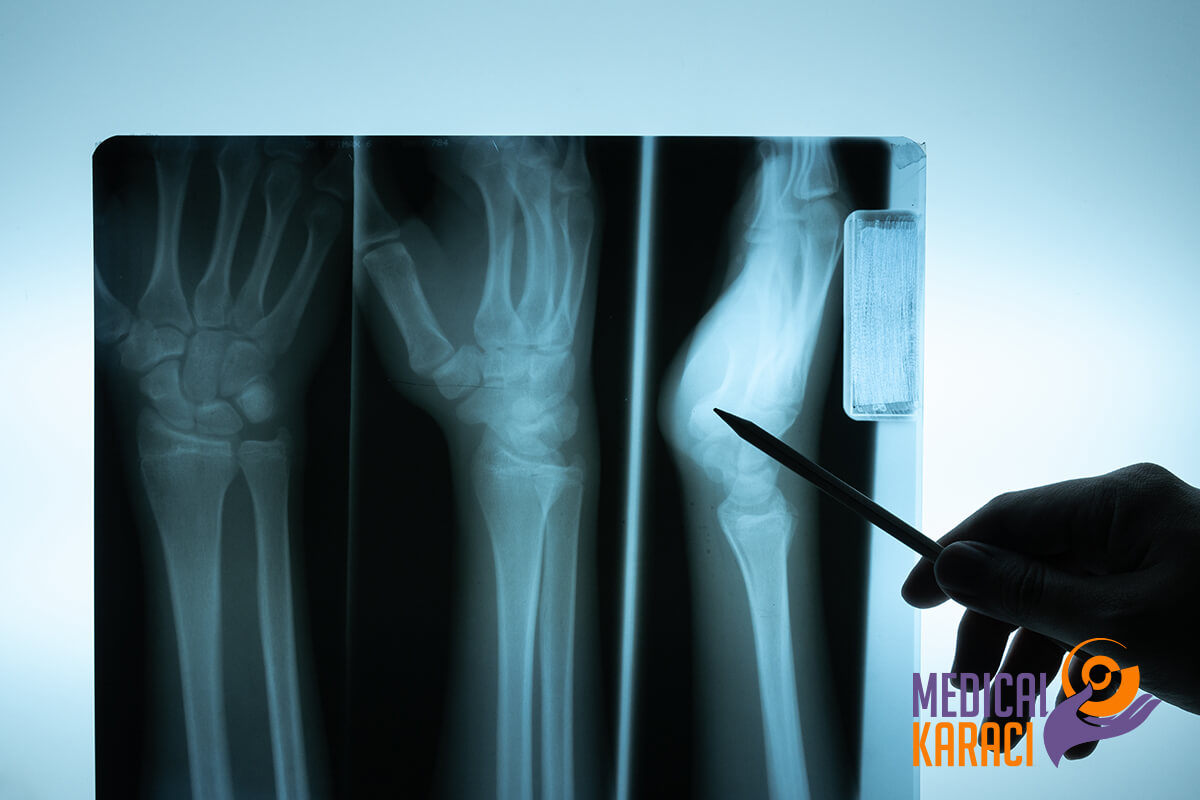
Diagnosis of rheumatic diseases
Establishing a diagnosis of systemic rheumatic disease requires integration of the patient's symptoms, physical examination findings, and diagnostic test results. When used with care, laboratory tests can be very specific and help greatly in establishing a correct diagnosis. The basis of early screening is to determine the erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP), which are both parts of the acute phase response. Clinicians sometimes rely heavily on objective indicators such as the presence or absence of autoantibodies. Few diagnostic tests are highly sensitive, although antinuclear antibody in systemic lupus erythematosus (SLE) and erythrocyte sedimentation rate in temporal arteritis are notable exceptions. Conversely, few diagnostic tests are highly specific; anti-proteinase-3 and anti-myeloperoxidase antibodies (types of antineutrophil cytoplasmic antibodies) in patients with Wegener's granulomatosis (and related vasculitides) and anti-double-chain and anti-Smith antibodies in lupus patients may be particularly useful in the right clinical setting because of their high specificity. Anti-citrullinated cyclic protein (anti-CCP), a newly described autoantibody that may be highly specific for rheumatoid arthritis, requires further investigation as its utility in clinical practice is uncertain.
Most rheumatologic diagnoses are made by effective history taking and physical examination rather than by examination.
Systemic symptoms, such as weight loss, anorexia and fever, point to systemic diseases such as rheumatoid arthritis, other polyarthritides, systemic lupus erythematosus, polymyalgia and vasculitis. Joint swelling is a symptom commonly reported by patients without objective evidence of it on examination. Inflammatory arthropathies should not be diagnosed unless the physician is able to objectively identify swelling, if necessary by arranging a rapid examination during an active episode. Diagnostic criteria for systemic rheumatic diseases are useful in guiding the collection of a history to verify a presumptive diagnosis.
Treatment of rheumatic diseases
For the treatment of rheumatic diseases, various types of drugs are prescribed. Some medicines only treat symptoms such as pain and inflammation, while others can change the course of the disease.
Depending on the condition, medical treatment may include:
- Oral analgesics (painkillers) such as acetaminophen and opioids such as oxycodone and hydrocodone, which do not affect the underlying cause of the disease
- Local analgesics
- Nonsteroidal anti-inflammatory drugs including ibuprofen and naproxen sodium, over-the-counter medicines, and prescription medicines called COX-2 inhibitors, which can help reduce pain and inflammation
- Corticosteroids, which have strong anti-inflammatory properties but significant side effects with prolonged use
- Disease-modifying antirheumatic drugs that can help slow the progression of rheumatic diseases by affecting the body's immune responses and inflammatory processes
- Biological agents that act by targeting specific steps in the body's inflammatory processes
- Janus kinase inhibitors, which work by targeting Janus kinase pathways that are involved in the body's immune system response
Other treatments for rheumatic diseases:
In addition to medications, a variety of other treatments may be prescribed for rheumatic diseases, including:
- Specific exercise regimens to increase muscle strength and joint flexibility
- Physiotherapy
- Occupational therapy
- Cryotherapy
- Heat Treatment
- Splints, braces and support devices for weak joints
- Relax therapy
- Surgery (especially for arthritis)
Patients with rheumatic diseases can live a full life if they are diagnosed on time and strictly follow their therapeutic regimen in close collaboration with their doctor.
Contact the consultants of ZIC "Medical Karaj" for more information.
Hospitals in this area
- Jean-Violette Medical Centre
- Acıbadem Mehmet Ali Aydınlar Atakent University Hospital
- Chorlu Watan Multidisciplinary Private Hospital
- Acıbadem Kozyatağı Hospital
- Acıbadem Taksim Hospital
- Medical Park Hospital, Bursa
- Acıbadem International Hospital
- Medipol Mega
- Medical Park Hospital, Trabzon city
- Istinye University Hospital, Medical Park, Gaziosmanpasa, Istanbul
- Medical Park, Ankara city
- Medical Park Hospital, Bahceliyevler, Istanbul
- VM Medical Park Hospital, Floria, Istanbul
- Liv Hospital
- Medical Park Hospital, Ordu
- Medical Park, Gebze
- Acıbadem Kayseri Hospital
- Acıbadem Bodrum Hospital
- Acıbadem Bakırköy Hospital Istanbul
- Acıbadem Maslak Hospital
- BHT CLINIC
- Acıbadem Hospitals Group
- Acıbadem Ankara Hospital
- Medical Park, Batman City
- Acıbadem Bursa Hospital
- Medical Park Hospitals Group
- Istinie University Hospital, Istanbul
- VM Medical Park Hospital, Pendik, Istanbul
- Acıbadem Altunizade Hospital
- Acıbadem Dr. Şinasi Can (Kadıköy) Hospital
- American Hospital
- Acıbadem Fulya Hospital
- Acıbadem Kocaeli Hospital
- Acıbadem Eskişehir Hospital
- Acıbadem Hospital Adana
- Medical Park Hospital, Gaziantep city
For more information, you can call +359895770869.