The field of neurosurgery is a medical specialty that deals with the diagnosis and treatment of patients with injuries or diseases/disorders of the brain, spinal cord, spinal column and peripheral nerves in all parts of the body. Neurosurgeons can work with patients of all ages, from premature infants to the elderly. Depending on the nature of the injury or illness, a neurological surgeon may provide surgical and/or non-surgical care.
Neurosurgery specialists are not just brain surgeons. They are medical specialists in neurosurgery who can also help patients suffering from back and neck pain, as well as a host of other ailments ranging from trigeminal neuralgia to head trauma and Parkinson's disease.
Neurosurgery is one of the most advanced disciplines in the world of science and medicine and involves the use of some of the most advanced technologies currently available. Increasingly, neurosurgery is using minimally invasive procedures that achieve comparable or better results than open surgery. Patient benefits include less pain, faster recovery and minimal scarring.
The main subspecialties of neurosurgery are:
- Pediatric neurosurgery - includes facial anomalies, spinal birth defects and tumors
- Neuro-oncology - treatment of brain and spinal tumours
- Functional neurosurgery - treating a range of conditions including epilepsy, movement disorders and cerebral palsy
- Neovascular surgery - including complex aneurysms and abnormal or narrowed blood vessels
- Traumatology - for the treatment of head injuries
- Cranial surgery - for skull base disorders and skull base tumors
- Spinal surgery
Some of the main types of conditions that neurosurgeons treat:
- tumours of the brain, spine and skull
- head and spinal cord injuries
- degenerative spine conditions and disc herniations
- vascular diseases of the spinal cord
- cerebral aneurysms and arteriovenous
- hemorrhagic and ischemic strokes
- epilepsy
- infections
- movement disorders such as Parkinson's disease
- certain mental disorders
- congenital conditions such as spina bifida
- conditions that affect the cerebrospinal fluid such as hydrocephalus
- pituitary tumors and neuroendocrine disorders
Research methods in the field of neurosurgery:
Neuroelectrophysiology
- Electroencephalogram (EEG) is a record of brain activity. During the test, tiny sensors are attached to the scalp to pick up the electrical signals generated when brain cells send messages. These signals are recorded by a machine and later examined by a doctor to see if they are abnormal.
- Electromyography (EMG) e test that measures the electrical activity of muscles and provides information about the muscular and nervous system. An EMG is performed at the same time as another test that gives information about the conduction function of nerves - electroneurography. In some cases, only electroneurography is performed. In electromyography, small sterile needle electrodes are inserted into the muscles to measure the electrical activity of the muscles and nerves. In electroneurography, the peripheral nerves are stimulated with short electrical impulses leading to muscle contraction.
- Challenged Potential Tests (EP) - measure the time it takes the brain to respond to sensory stimulation by light, sound or touch. They are used as a diagnostic tool and can detect abnormal responses to stimulation that may indicate disease.
Neuroradiology
- Radiography - a method of imaging organs in the human body using a low dose of X-rays. It is used for diagnostic purposes in various diseases.
- Scanner - a modern diagnostic method with X-rays that provides slice images of internal organs and structures. There is almost no field of medicine in which CT is not widely used in the diagnostic process.
- Magnetic resonance imaging - a medical imaging technique that uses a magnetic field and computer-generated radio waves to create detailed images of organs and tissues in the body.
Neuroophthalmology
Accurate diagnosis and follow-up of the eye condition is essential for a correct neurological diagnosis.
Otoneurology
Correct diagnosis of inner ear diseases is of great importance for neurological diagnosis.
Diagnostic invasive methods/manipulations in neurosurgery:
- Puncture techniques for taking liquor - (lumbar puncture)
The human brain normally "floats" in so-called liquor or cerebrospinal fluid. The liquor cushions and protects the brain from damage during various head movements or impacts. It also supplies brain tissue with important nutrients, growth factors and hormones. Lumbar puncture is a procedure in which a small amount of liquor is withdrawn in order to be examined for changes that are seen in various diseases. Lumbar puncture is performed at the level of the third and fourth lumbar vertebrae or at the level of the fourth lumbar and first sacral vertebrae. For the purpose of the examination, usually about 10 ml of liquor is taken.
- Cerebral blood flow studies:
- Doppler - Doppler sonography is a harmless and painless method for examining the direction and velocity of blood flow in blood vessels (arteries and veins). Its basis is the Doppler effect, which is a change in the frequency of ultrasound waves from the moving form elements of the blood, mostly from red blood cells.
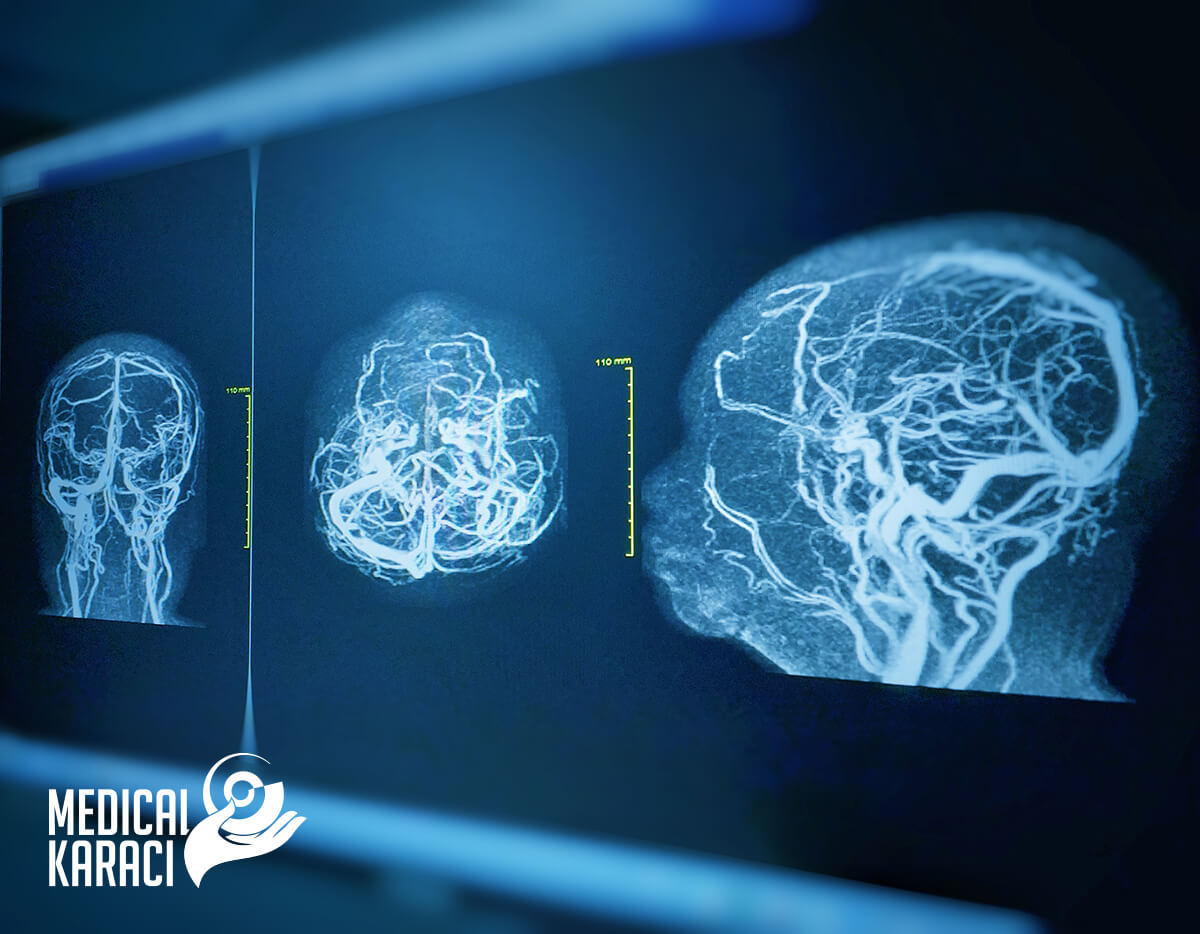
- Angiography - X-rays and contrast are used to obtain images of the intraluminal space of the arteries and veins of the brain and spinal cord.
Operative techniques performed in the field of neurosurgery:
Brain surgery
Removal of clots
Surgical thrombectomy is a type of surgery to remove a blood clot from inside an artery or vein. Usually, blood flows freely through the blood vessels- the arteries and veins. Arteries carry blood rich in oxygen and nutrients to the body. Veins carry waste products back to the heart. In some cases, the blood thickens and a blood clot forms in one of these vessels. This can block blood flow. When blood flow is blocked, nearby tissues can be damaged. During a surgical thrombectomy, an incision is made in the blood vessel, the clot is removed, and the blood vessel is repaired. This restores blood flow. In some cases, a balloon may be inserted into the blood vessel to keep it open.
Repair of aneurysm
An aneurysm is an abnormal enlargement of a blood vessel that is due to a defect in the vessel wall. The condition can develop in any blood vessel, but is most commonly seen in the abdominal aorta and brain. In most cases, a cerebral aneurysm is asymptomatic for a long time. In rare cases, the pathological dilation of the blood vessel may rupture and intracerebral hemorrhage may occur. This can lead to stroke, varying degrees of brain damage or death. Two are the most common treatments for cerebral aneurysm:
- Surgical clipping - this is a procedure whose purpose is to remove the enlargement of the blood vessel wall. After penetrating the skull, the surgeon places a small clip at the base of the aneurysm and thus stops the blood flow to it.
- Endovascular prosthetics - this procedure is less invasive. In it, the surgeon inserts a small tube - a catheter through a large artery, most often in the groin area and through this tube reaches the desired artery in the brain where the aneurysm is located. He then passes a platinum wire through the catheter, which is wound in the form of a spiral at the base of the aneurysm and thus stops the flow of blood to the pathological enlargement of the blood vessel wall.
Tumour removal
Surgery is one of the main treatments for brain and spinal cord tumors. Surgery can be done for:
- removal of the entire tumor,
- removing part of the tumour to slow its growth and affect symptoms
- drainage of fluid into the brain in hydrocephalus
- brain tumour diagnosis - biopsy
Brain surgery is not right for every patient. It is a complex operation that is not always possible. Some tumours, for example, grow in areas of the brain that are difficult for doctors to operate on, such as the brain stem, for example.
Stopping brain bleeding
Hemorrhage in the brain is a type of stroke. It is caused by an artery bursting in the brain and causing localized bleeding into surrounding tissues. This bleeding kills brain cells. There are several risk factors and causes for brain hemorrhages. The most common include:
- Head trauma.
- High blood pressure.
- Aneurysm.
- Abnormalities of blood vessels. (Arteriovenous malformations) Weaknesses in the blood vessels in and around the brain may be present at birth and only diagnosed if symptoms develop.
- Amyloid angiopathy. This is an abnormality of the walls of blood vessels that sometimes occurs with aging and high blood pressure. It can cause many small, unnoticed hemorrhages before causing a large one.
- Blood or bleeding disorders. Hemophilia and sickle cell anemia can contribute to lower blood platelet levels and clotting. Blood thinners are also a risk factor.
- Liver disease. This condition is associated with increased bleeding in general.
- Brain tumors.
Symptoms of cerebral haemorrhage can vary. They depend on the site of bleeding, the severity of bleeding and the amount of tissue affected. Symptoms develop suddenly. They may gradually get worse.
Symptoms include:
- Sudden severe headache
- Seizures with no previous history of seizures
- Weakness in the arm or leg
- Nausea or vomiting
- Reduced alertness, lethargy
- Changes in vision
- Numbness or tingling
- Difficulty speaking or understanding speech
- Difficulty swallowing
- Difficulty writing or reading
- Loss of fine motor skills
- Loss of coordination
- Loss of balance
- Abnormal taste sensations
- Loss of consciousness
How is cerebral haemorrhage treated?
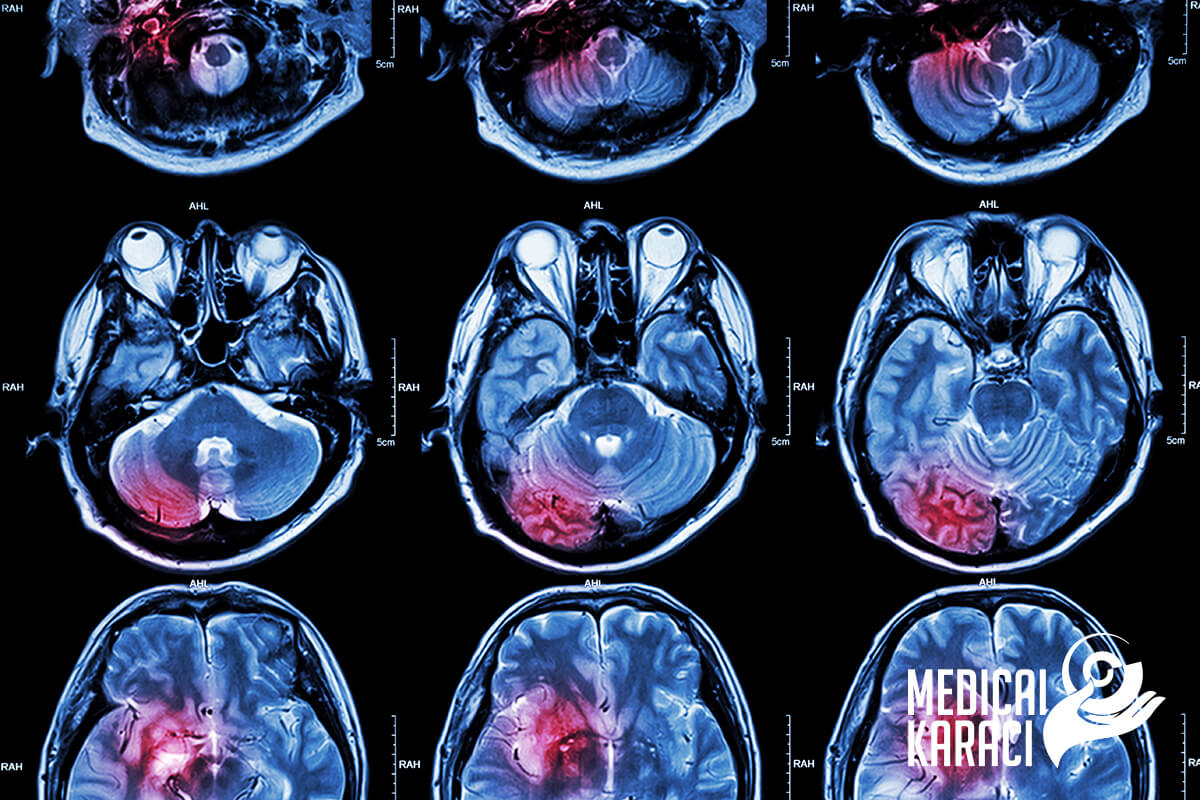
Doctors may conduct various imaging tests, such as a CT scan, which can reveal internal bleeding or blood build-up, or an MRI. A neurological examination or an eye examination may also be performed, which may show swelling of the optic nerve. A lumbar puncture is not usually performed as it can be dangerous and worsen the situation. The treatment of bleeding in the brain depends on the location, cause and extent of the hemorrhage. Surgery may be needed to relieve the swelling and prevent bleeding. Certain medications may also be prescribed. These include painkillers, corticosteroids or osmotics to reduce swelling and anticonvulsants to control seizures.
Treatment of craniocerebral trauma
A variety of treatments can help a person recover from a craniocerebral injury and can sometimes reduce or eliminate some of the physical, emotional and cognitive problems associated with the injury. The specifics of treatment, including the type and duration, depend on how severe the injury is and the area of the brain that was traumatized.
Mild craniocerebral trauma, sometimes called a concussion, may not require specific treatment other than rest. However, it is very important to follow specialists' instructions for complete rest and a slow return to normal activities after a mild craniocerebral injury. If a person returns to normal activities too soon and begins to experience symptoms, the healing process can take much longer. Some activities, such as computer work and concentration, can fatigue the brain even though they are not physically taxing. A person with a concussion may need to reduce these types of activities or take frequent breaks to let the brain rest. In addition, alcohol and other drugs can slow recovery and increase the chances of re-injury.
Emergency care for craniocerebral trauma usually focuses on stabilizing and keeping the patient alive, including ensuring that the brain receives enough oxygen, controlling blood and brain pressure, and preventing further injury to the head or neck. Sometimes surgery is needed as part of emergency care to reduce brain damage. Surgery may include:
- Removal of blood clots. Bleeding in the brain or between the brain and skull can cause large areas of clotted blood, called hematomas. These areas of clotted put pressure on the brain and can damage brain tissues
- Repair of skull fractures. Identifying severe skull fractures or removing pieces of skull or other debris from the brain area can help begin the healing process of the skull and surrounding tissues.
- Relief of pressure inside the skull. The increased pressure from swelling, blood and others inside the skull, damage the brain. In some cases, it is necessary to make a hole in the skull or to make a shunt or drain to relieve the pressure inside and allow the excess fluid to drain out.
Ventriculoperitoneal shunt
A ventriculoperitoneal shunt is a medical device that relieves pressure on the brain caused by fluid build-up.
Shunting is a surgical procedure that primarily treats a condition called hydrocephalus. This condition occurs when excess cerebrospinal fluid collects in the ventricles of the brain. The cerebrospinal fluid softens the brain and protects it from injury in the skull. Normally, cerebrospinal fluid flows through the ventricles to the base of the brain. The fluid then bathes the brain and spinal cord before being reabsorbed into the blood. When this normal flow is disrupted, the build-up of fluid can create damaging pressure on the tissues of the brain, which can damage it. Doctors surgically place a ventriculoperitoneal shunt in one of the brain's ventricles to divert the fluid and restore the normal flow and absorption of cerebrospinal fluid.
Stereotactic radiosurgery
Stereotactic radiosurgery is a very precise form of therapeutic radiation that can be used to treat abnormalities in the brain and spine, including cancer, epilepsy, trigeminal neuralgia, and arteriovenous malformations.
Stereotactic radiosurgery does not involve an incision or opening. During the procedure, X-rays are carefully directed at the abnormal tissues through the skin from different directions.
Radiosurgery works in the same way as other types of therapeutic radiology: X-rays distort or destroy the DNA of cells in abnormal areas so they cannot reproduce and grow. With optimal treatment, the abnormal tissue becomes inactive and gradually shrinks.
The surgical precision of the technique is particularly useful in treating small or hard-to-reach abnormalities in the brain and spine. The targeted focus of radiation in radiosurgical techniques results in less damage to healthy surrounding tissue and less risk of infection, making it safer for those who have just undergone surgery.
Stereotactic radiosurgery causes fewer and milder side effects than conventional radiotherapies, which cover a wider area and can affect healthy tissue. The following side effects are usually temporary and improve within a few weeks.
- fatigue
- skin irritation at the treatment site
- hair loss at the treatment site
- главоболие
- neurological symptoms such as numbness or weakness
- gastrointestinal symptoms such as nausea, vomiting or diarrhea
Stereotactic radiosurgery has a team approach involving specialists in radiation oncology and neurosurgery. A dosimetry expert determines how the beams should be directed and a physicist calculates the amount of radiation the patient should receive, balancing risk and potential effectiveness. A key element in planning the procedure is maximizing treatment to the abnormal tissues while protecting the healthy tissues surrounding the abnormal area.
Endovascular procedures
Carotid endarterectomy
Carotid endarterectomy is a procedure to treat carotid artery disease. This disease occurs when fatty deposits build up in one of the carotid arteries. The carotid arteries are blood vessels located on each side of the neck. This build-up of plaque (atherosclerosis) can restrict blood flow to the brain. Removing the plaque causing narrowing of the artery can improve blood flow in the carotid artery and reduce the risk of stroke.
In carotid endarterectomy, local or general anesthesia is administered. An incision is made along the front of the neck, the carotid artery is opened, and the plaques that obstruct the artery are removed. The surgeon then repairs the artery with stitches or a patch.
Sometimes surgeons may use another technique called carotid endarterectomy eversion. This involves cutting the carotid artery and turning it inside out, then removing the plaque. The surgeon then reattaches the artery. Doctors may recommend carotid endarterectomy if there is severe narrowing of the carotid artery. There are several other factors that will be considered besides the degree of blockage of the artery.
If carotid endarterectomy is not the best option for the patient, a procedure called carotid angioplasty and stenting can be performed instead of carotid endarterectomy. In this procedure, doctors insert a long hollow tube (catheter) with a small balloon attached through a blood vessel in the neck to a narrowed artery. The balloon is then inflated to dilate the artery. Often a metal mesh tube (stent) is put in to reduce the chance of the artery narrowing again.
Embolization of cerebral aneurysms
Embolization of a cerebral aneurysm involves inserting a catheter into the femoral artery in the patient's leg and passing the catheter through the vasculature into the patient's head and up to the aneurysm. The entire process is performed using continuous X-ray imaging and high-speed radiographic imaging techniques.
Once the doctor has discovered the presence, size, and location of the aneurysm, a smaller "microcatheter" is placed inside the original catheter. When the microcatheter is successfully navigated into the aneurysm opening, the coiling system is put in place. The platinum coils are deposited into the aneurysm, reducing or blocking blood flow. The coils are made of platinum so that they are visible by X-ray and are flexible enough to conform to the shape of the aneurysm. The purpose of coiling is to pack the aneurysm tightly to shut off blood flow to the aneurysm, thus preventing it from rupturing. Once inserted into the aneurysm, a small electric current is passed through the electrical wire. As a result of this electrolysis, the coil detaches from the wire and remains inside the aneurysm. Once the aneurysm is packed, the catheters are removed. Coiling procedures are performed under general anesthesia.
When a patient is diagnosed with a brain aneurysm, timing is critical. There is a 50 % chance of mortality and morbidity after the first rupture of the aneurysm. This number increases to 75 % after a second rupture.
Surgery of peripheral nerves
Carpal tunnel release
Carpal tunnel release is an operation used to treat the painful condition known as carpal tunnel syndrome. Doctors believed that carpal tunnel syndrome was caused by excessive trauma or repetitive motion performed by the wrist or arm, often during work. It is now known that it is most likely a congenital predisposition - some people simply have smaller carpal tunnels than others. Carpal tunnel syndrome can also be caused by injury, such as a sprain or fracture, or repetitive use of a vibrating tool. It is also associated with pregnancy, diabetes, thyroid disease and rheumatoid arthritis.
The median nerve and tendons that allow the fingers to move pass through a narrow passage in the wrist called the carpal tunnel. The carpal tunnel is formed by the bones of the wrist and the transverse carpal ligament across the top of the wrist. When this part of the body is injured or tight, swelling of the tissues in the tunnel can pinch the median nerve. This causes numbness of the hand, pain and loss of function if left untreated. Symptoms usually start slowly and can worsen over time.
Carpal tunnel release is usually an outpatient procedure. There are 2 types of carpal tunnel release surgery. The traditional method is the open release, in which the surgeon cuts the wrist to perform the operation.
The other method is endoscopic carpal tunnel release, in which a thin, flexible tube containing a camera is inserted into the wrist through a small incision. The camera guides the doctor as the surgery is performed with thin instruments inserted into the wrist through another small incision.
Ulnar nerve release
Ulnar nerve release surgery is a procedure for cubital tunnel syndrome. Cubital tunnel syndrome is a condition in which nearby tissue puts pressure on a nerve in the cubital tunnel, a narrow space through which the ulnar nerve passes around the elbow.
Similar to the surgery performed for carpal tunnel syndrome, ulnar nerve release surgery helps reduce pressure on the nerve by cutting and dividing the upper ligament. The ligament may gradually regrow after surgery, but there will be more room in the ulnar tunnel.
Stimulation of the vagus nerve
Stimulation of the vagus nerve involves the use of an electrical pulse stimulation device. There is one vagus nerve on each side of the body, running from the brainstem through the neck to the chest and abdomen.
In conventional vagus nerve stimulation, a device is surgically implanted under the skin of the chest, and a wire is inserted under the skin connecting the device to the left vagus nerve. When activated, the device sends electrical signals along the left vagus nerve to the brainstem, which then sends signals to specific areas in the brain. The right vagus nerve is not used because it is more likely to carry fibers that deliver impulses to the heart.
New, non-invasive vagus nerve stimulation devices that do not require surgical implantation have been approved in Europe for the treatment of epilepsy, depression and pain.
Spine surgeries
Discectomy
A discectomy is the surgical removal of part or all of an intervertebral disc. Discectomy is resorted to in the presence of disc herniation when non-operative treatment does not work.
Discectomy is performed under general anesthesia. Different methods are used to remove the intervertebral disc:
- open discectomy - 7-9 cm incision
- microdiscectomy - 4-5 cm incision.
- endoscopic microdiscectomy
With a diskectomy, there is little chance of a recurrent disc herniation in the segment as most of the disc is removed.
Laminectomy
A laminectomy is an operation that creates space by removing the lamina, the back part of the vertebra that covers the spinal canal. Also known as decompression surgery, a laminectomy widens the spinal canal to relieve pressure on the spinal cord or nerves.
Spinal fusion
Spinal fusion is an operation to permanently connect two or more vertebrae in the spine, eliminating movement between them.
Vertebroplasty and kyphoplasty
Vertebroplasty and kyphoplasty common surgical techniques for the treatment of spinal compression fractures. Vertebroplasty involves percutaneous injection of bone cement into the spongy bone of the vertebral body to relieve pain and prevent further loss of vertebral height. Kyphoplasty uses an inflatable balloon to create a cavity for the cement with the additional potential goals of restoring height and reducing kyphosis. Vertebroplasty and kyphoplasty are effective treatment options and reduce pain associated with vertebral body fractures. Biomechanical studies have shown that kyphoplasty is initially better at increasing vertebral height and reducing kyphosis, but these results are lost with repetitive loading. Complications secondary to cement extravasation include compression of neural elements and venous embolism. These complications are rare but more common in vertebroplasty. Vertebroplasty and kyphoplasty are safe and effective procedures for the treatment of spinal compression fractures.
Stabilization and reconstruction of the spine
Spinal reconstruction surgery can be life-saving for patients with deformities or dislocations affecting part of the spine. During the procedure, one or more vertebrae may be removed from the spine and replaced with artificial implants or a bone graft to align and stabilize the spine
Thanks to high-quality technology, the risk in neurosurgical operations is minimized:
Neuronavigation:
Cerebral, spinal and neurosurgicalinterventions are performed with the Neuronavigation system, which enables high-quality three-dimensional visualization. This method is applied in the presence of brain tumors, brain tumor biopsy, spine and spinal cord surgery. Neuronavigation is a system that allows the images obtained before and during the patient's surgery to be used during surgical intervention. In this method, an MRI of the patient is taken before proceeding to surgery and the results are transferred to the neuronavigation device. The anatomical or physiological images obtained from the MRI can be used in the surgery. In this way, real-time neuronavigation is performed during the surgical intervention, through which the different risk areas in the patient's brain or spine can be seen and an action plan is drawn up accordingly. This technology provides a precision accuracy approach to approximate the target area of the brain or spine and minimizes potential damage to health tissues during surgery.
Neuromonitoring:
During operations on tumors located in sensitive areas of the brain, aneurysm or arteriovenous malformation, spinal tumors, and precision spinal surgeries (e.g., scoliosis), the neurosurgeon monitors the patient using signals from electrodes placed on the patient's face, arms, and legs before placing an anesthetic. When the signal is lowered, the doctor receives a warning that he is in a sensitive area. Thanks to this, the risk of paralysis occurring to the face, arm or leg is greatly reduced.
Intraoperative ultrasonography:
During the course of the operation, the radiologist uses an ultrasound machine to determine the location of the tumor and the extent of its removal. This allows for the complete removal of tumours that are difficult to distinguish from brain and spinal cord tissue.
Endoscopy:
Provides good visibility from a small area in areas where narrow penetration corridors are used, such as pituitary surgery, tumors inside the ventricle, and hydrocephalus. Furthermore, the method represents an alternative treatment to microsurgery for such common spinal problems as disc herniation.
Gliolan coloring technique:
Before surgery, the patient is given the preparation Gliolan, which provides a different staining of the tumor. During surgery, by applying a special filter to the surgical microscope, normal brain tissue and tumor tissue are stained in different colors. With this method, damage to healthy brain tissue is minimised and tumour removal is maximised. The risk of neurological loss in the patient is also reduced.
Awake craniotomy:
For precision surgery of tumors located in the speech center or in the area responsible for movement of the patient's arms and legs, also called the "motor area," the patient is operated on while awake. In this way, the patient's speech and movements of the arms and legs are controlled during the operation, thus preventing damage from occurring. This method increases the success rate of operations.
Intraoperative CT (O-Arm):
At the time of surgery, a CT scan is performed to visualize the current condition. It is mostly used in operations for implanting screws in the spine. There is no possibility of error in screw implantation operations performed with the O-Arm technology, which provides three-dimensional tomographic imaging. At every stage of the operation, the surgeon receives key information and the risk of recurrence is minimised. Thanks to this, the patient is exposed to less radiation. The method makes it possible to operate on smaller patients. Another advantage is the reduced risk of infection.
Hospitals in this area
- Acıbadem Ankara Hospital
- Medical Park Hospital, Bahceliyevler, Istanbul
- Yeditepe University Hospital
- VM Medical Park Hospital, Floria, Istanbul
- Istinye University Hospital, Medical Park, Gaziosmanpasa, Istanbul
- VM Medical Park Hospital, Pendik, Istanbul
- Medipol Mega
- Memorial Hospital, Kayseri
- Acıbadem Mehmet Ali Aydınlar Atakent University Hospital
- Acıbadem Kocaeli Hospital
- Medical Park, Gebze
- Memorial, Ataşehir, Istanbul
- Memorial Hospitals Group
- Lokman Hekim Hospital Istanbul
- Memorial Medstar Hospital, Topçular, Antalya
- Medical Park Hospital, Bursa
- BHT CLINIC
- Chorlu Watan Multidisciplinary Private Hospital
- Acıbadem Bursa Hospital
- University Hospital Koch
- Acıbadem Maslak Hospital
- Acıbadem Taksim Hospital
- American Hospital
- Reap Health Group
- Болница Хисар
- Memorial Hospital, Hizmet, Istanbul
- Okan University Hospital
- Acıbadem Hospitals Group
- Memorial Hospital, Ankara, Turkey
- Liv Hospital
- Medical Park Hospital, Trabzon city
- Memorial Hospital, Shishli, Istanbul
- Acıbadem Dr. Şinasi Can (Kadıköy) Hospital
- Medical Park Hospital, Gaziantep city
- Istinie University Hospital, Istanbul
- Memorial Hospital, Diyarbakir
- Acıbadem Eskişehir Hospital
- Wiener Privatklinik
- Medical Park, Ankara city
- Acıbadem Altunizade Hospital
- Acıbadem International Hospital
- Medical Park Hospital, Ordu
- Acıbadem Fulya Hospital
- Bahceliyevler Memorial, Istanbul
- Medical Park Hospitals Group
- Belt Hospitals
- Acıbadem Kayseri Hospital
- Memorial Medstar Hospital, Antalya
- Acıbadem Hospital Adana
- Memorial Hospital, city of Dijle
- Acıbadem Bodrum Hospital
- Memorial, Antalya, Turkey
- Medical Park, Batman City
- Acıbadem Bakırköy Hospital Istanbul
- Acıbadem Kozyatağı Hospital