Retinal detachment is a serious condition that can lead to vision loss if not treated in time.
What is retinal detachment?
A retinal detachment describes an abnormal situation in which a thin layer of tissue (the retina) at the back of the eye pulls away from its normal position. Retinal detachment separates the retinal cells from the layer of blood vessels that provides oxygen and nutrition to the eye. The longer retinal detachment goes untreated, the greater the risk of permanent vision loss in the affected eye.
The patient should seek immediate medical attention from a specialist if he notices any of the characteristic symptoms.
What are the symptoms of retinal detachment?
The retinal detachment itself is painless. But the warning signs almost always appear before the problem appears or is advanced, such as:
- The sudden appearance of many floating elements - tiny specks that seem to float across the field of view
- Flashes in one or both eyes
- Blurred vision
- Gradually reduced peripheral vision
- Curtain-like shadow over the field of vision
- When to see a doctor
Immediate medical attention should be sought if the signs or symptoms of retinal detachment are present. Retinal detachment is a medical emergency in which permanent vision loss can occur.
What are the causes of retinal detachment?
There are three different types of retinal detachment:
- Regmatogenous- these types of retinal detachments are the most common. Rhegmatogenous detachments are caused by a hole or tear in the retina that allows fluid to pass through it and collect under the retina. This fluid builds up and causes the retina to pull away from the underlying tissues. The areas where the retina detaches lose their blood supply and stop working, resulting in vision loss. The most common cause of rhegmatogenous detachment is aging. As we age, the gel-like material that fills the inside of the eye, known as the vitreous, can change consistency and shrink or become more fluid. Usually the vitreous detaches from the surface of the retina without any complications, a common condition called posterior vitreous detachment. One complication of this separation is a tear. As the vitreous detaches or detaches from the retina, it can pull on the retina with enough force to create a retinal tear. Left untreated, the liquid vitreous can pass through the tear into the space behind the retina, resulting in retinal detachment.
- Traction peeling- this type of detachment can occur when tissue grows over the surface of the retina, causing the retina to pull away from the back of the eye. Traction detachment is commonly seen in people who have poorly controlled diabetes or other conditions.
- Exudative- in this type of detachment, fluid accumulates under the retina, but there are no holes or tears in the retina. Exudative detachment can be caused by age-related macular degeneration, injury to the eye, tumors, or inflammatory diseases.
Risk factors
- The following factors increase the risk of retinal detachment:
- Ageing - retinal detachment is more common in people over 50
- Previous retinal detachment
- Family history of retinal detachment
- Extreme myopia (myopia)
- Previous eye surgery, such as cataract removal
- Previous severe eye injury
- Previous other eye disease or disorder, including uveitis or peripheral retinal thinning
How is detachment diagnosedon the retina?
A detailed eye examination is needed to diagnose retinal detachment. The doctor may recommend other tests after the dilated eye examination. These tests are non-invasive and may include:
- Optical coherence tomography (OCT)
- Imaging of the ocular fundus
- Ocular ultrasound
- CT scan- this imaging test is usually used if there is a history of trauma or possible penetrating injury to the eye.
How is retinal detachment treated?
The ophthalmologist will discuss treatment options with you. You may need a combination of treatments for best results. Treatments include:
- Laser therapy or cryopexy
- Pneumatic retinopexy
- Scleral buckle
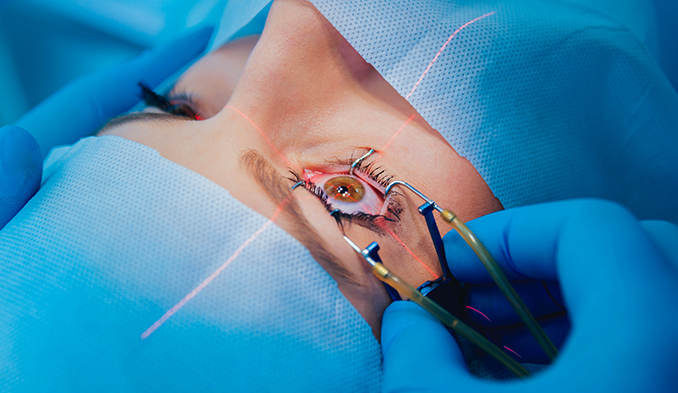
- Vitrectomy
Laser therapy or cryopexy
There are cases in which the eye doctor can diagnose a retinal tear before the retina begins to recede. The doctor may use a medical laser or freezing instrument to seal the tear. These devices create a scar that holds the retina in place.
Pneumatic retinopexy
During pneumatic retinopexy, the doctor injects a small gas bubble into the eye.
The balloon squeezes the retina, closing the tear.
A laser or cryopexy may need to be applied to seal the tear. The body reabsorbs the fluid collected under the retina and it can now stick to the eye wall the way it should. Eventually the body also absorbs the gas bubble. After surgery, the doctor makes recommendations for keeping the head still for a few days and position in a certain posture to promote healing. These recommendations may seem uncomfortable or tedious, but are especially important. This is a short-term sacrifice for long-term benefits.
Scleral buckle
During scleral buckle surgery, the doctor surgically places a silicone band or sponge (buckle) around the eye. The tape holds the retina in place and stays there permanently. The tear is sealed with a laser or cryopexy. The doctor may inject a gas bladder or drain fluid under the retina to help reattach it.
Vitrectomy
During a vitrectomy, the doctor surgically removes the vitreous and uses a laser or freezing to seal any tears or holes in the retina. He inserts a bubble of air, gas, or silicone oil into the eye to put the retina back in place.
If the doctor uses silicone, you will remove it a few months later. The body reabsorbs gas and air bubbles, and in this case there is no need for removal. If you have a gas bladder, you may need to avoid activities at certain heights. Changing altitude can increase the size of the gas bubble and the pressure in the eye. You will need to avoid flying and traveling to high altitudes for a period of time.
Complications/side effects of retinal detachment treatment
Although retinal reattachment surgery is often very successful, any surgery can have risks or complications. These risks and complications include:
- Bleeding
- Infection
- Higher pressure in the eye
- The possibility of needing another operation
- Appearance of epiretinal membrane
- Rapid cataract formation requiring additional surgery
What can I expect after retinal detachment surgery?
After treatment of a detached retina, there may be some discomfort that may last for several weeks. The doctor will recommend painkillers and other forms of relief and will say when you can exercise, drive and return to your normal activities.
What else you can expect after surgery:
- Eye patch: Wear the eye patch for as long as your doctor tells you to.
- Head position: if a balloon is placed in the eye, follow the instructions for the head position. The doctor will show what position the head should be in and how long to hold it there to help heal your eye.
- Eye drops: the doctor will instruct you how to use the drops to help the eye recover.
- Improved vision: About four to six weeks after surgery, you will start to notice that your vision is improving. It may take several months until you notice the full effect after surgery. The sooner the surgery is done, the better results can be expected.
Contact the coordinators of the Medical Center if you need surgery for retinal detachment. We will refer you to the right specialists!