When you have a blocked tear duct, tears can't drain normally, which creates a watery and irritated eye. The condition is caused by a partial or complete blockage of the tear drainage system.
A blocked tear duct is common in newborns. The condition usually improves without any treatment during the first year of life. The incidence of acquired nasolacrimal duct obstruction increases with age. In adults, the obstructed lacrimal duct may be due to injury, infection or rarely a tumor.
Diagnosing
To diagnose your condition, the doctor talks about your symptoms, examines your eyes and does several tests. An examination is made inside the nose to determine if there are any structural disorders of the nasal passages that are causing the blockage. If your doctor suspects a blocked tear duct, other tests may be necessary to find the location of the blockage.
Tests used to diagnose a blocked tear duct include:
Tear drainage test.
This test measures how quickly tears drain. One drop of a special dye is placed on the surface of each eye. You may have a blocked tear duct if, after five minutes, most of the dye is still on the surface of your eye.
Irrigation and drilling.
The doctor may flush saline through the tear drainage system to check how well it drains. He may insert a thin instrument, a probe, through the small drainage holes in the corner of your eyelid to check for blockages. In some cases, this examination may even solve the problem.
Eye imaging tests.
For these procedures, a contrast dye is passed from a point in the corner of your eyelid through the tear drainage system. An X-ray, computed tomography (CT) scan, or magnetic resonance imaging (MRI) is then used to determine the location and cause of the blockage.
Treatment
Treatment depends on what is causing the blocked tear duct. You may need more than one approach to correct the problem. If a tumor is causing the tear duct blockage, treatment will focus on the cause of the tumor. Surgery may be performed to remove the tumor or other treatments may be recommended to reduce it. If an infection is present, antibiotic eye drops or pills may be prescribed.
If you have had a facial injury that caused a tear duct blockage, you may wait a few months to see if the condition improves until the injury heals. As the swelling reduces, your tear ducts may unclog on their own.
Expansion and drilling.
In infants, this technique is performed under general anesthesia. The doctor dilates the punctal holes with a special dilating instrument and inserts a thin probe through the punctum and into the tear drainage system. In adults with a partially constricted punctum, the doctor may dilate the punctum with a small probe and then flush (irrigate) the tear duct. This is a simple outpatient procedure that often provides at least temporary relief.
Stenting or intubation.
This procedure is usually performed under general anesthesia. A thin tube made of silicone or polyurethane is passed through one or both points at the corner of the eyelid. These tubes are then passed through the tear drainage system into your nose. A small loop of tubing will remain visible in the corner of your eye. The tubes are usually left in for about three months before being removed. Possible complications include inflammation from the presence of the tube.
Balloon catheter dilation.
If other treatments have not worked or the blockage recurs, this procedure can be used. It is usually effective in infants and young children and can also be used in adults with partial blockage. General anesthesia is first administered to the patient. The doctor then passes a tube (catheter) with a deflated balloon at the tip through the tear duct blockage into the nose. The doctor inflates and deflates the balloon several times to open the blockage.
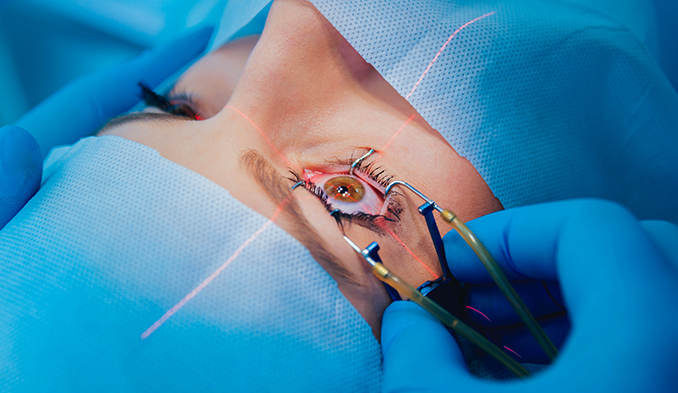
Surgery
The surgery commonly used to treat blocked tear ducts is called a dacryocystorhinostomy. This procedure opens the tear duct. It is performed under general anesthesia or local anesthesia if performed as an outpatient procedure. The steps in this procedure vary depending on the exact location and extent of the blockage, as well as the surgeon's experience and preference.
External method.
In external dacryocystorhinostomy, the surgeon makes an incision on the side of the nose, near the lacrimal sac. After connecting the lacrimal sac to the nasal cavity and placing a stent in the new passage, the surgeon closes the skin incision with several sutures.
Endoscopic or endonasal.
In this method, the surgeon uses a microscopic camera and other small instruments inserted through the nasal opening to the canalicular system. This method does not require an incision, so it leaves no scar. But the success rate is not as high as with the external procedure.
After surgery, a nasal decongestant spray and eye drops are used to prevent infection and reduce inflammation. After 6 to 12 weeks, any stents used to keep the new canal open during the healing process are removed.
The procedure is safe for the treatment of congenital, traumatic and primary acquired nasolacrimal duct obstruction. The advantage is that it leaves no scar and preserves the medial structures. It can be performed successfully as a unilateral and bilateral procedure.
Dacryocystorhinostomy has a high success rate (80%-100%) with a low complication rate (1%-6%).